
Human papillomavirus (HPV) infects 13 million people – including teens – each year. While nine out of every 10 HPV infections resolve on their own, some people carry the virus for longer periods of time and can develop cancer or precancerous conditions. Each year, 36,000 cases of cancer develop because of HPV infection.
There is a way to prevent these cancers: the HPV vaccine is safe and effective – and can prevent more than 90% of cancers from ever developing. Since being introduced more than 15 years ago, research has shown that the types of HPV infections that cause most cancers have dropped 88% among teen girls.
Despite the vaccine’s proven effectiveness, public acceptance of the vaccine as part of routine immunizations continues to lag. These are some of the most common myths about the HPV vaccine.
Myth: HPV is uncommon.
Fact: HPV is very common – nearly everyone will get HPV during some point in their lives. More than 42 million people living in the U.S. today have the virus.
The virus is spread through close skin-to-skin contact, including vaginal, anal or oral sex. Often, HPV presents no symptoms in the infected person, and this is why it is so important for all men and women to have appropriate cancer screenings.
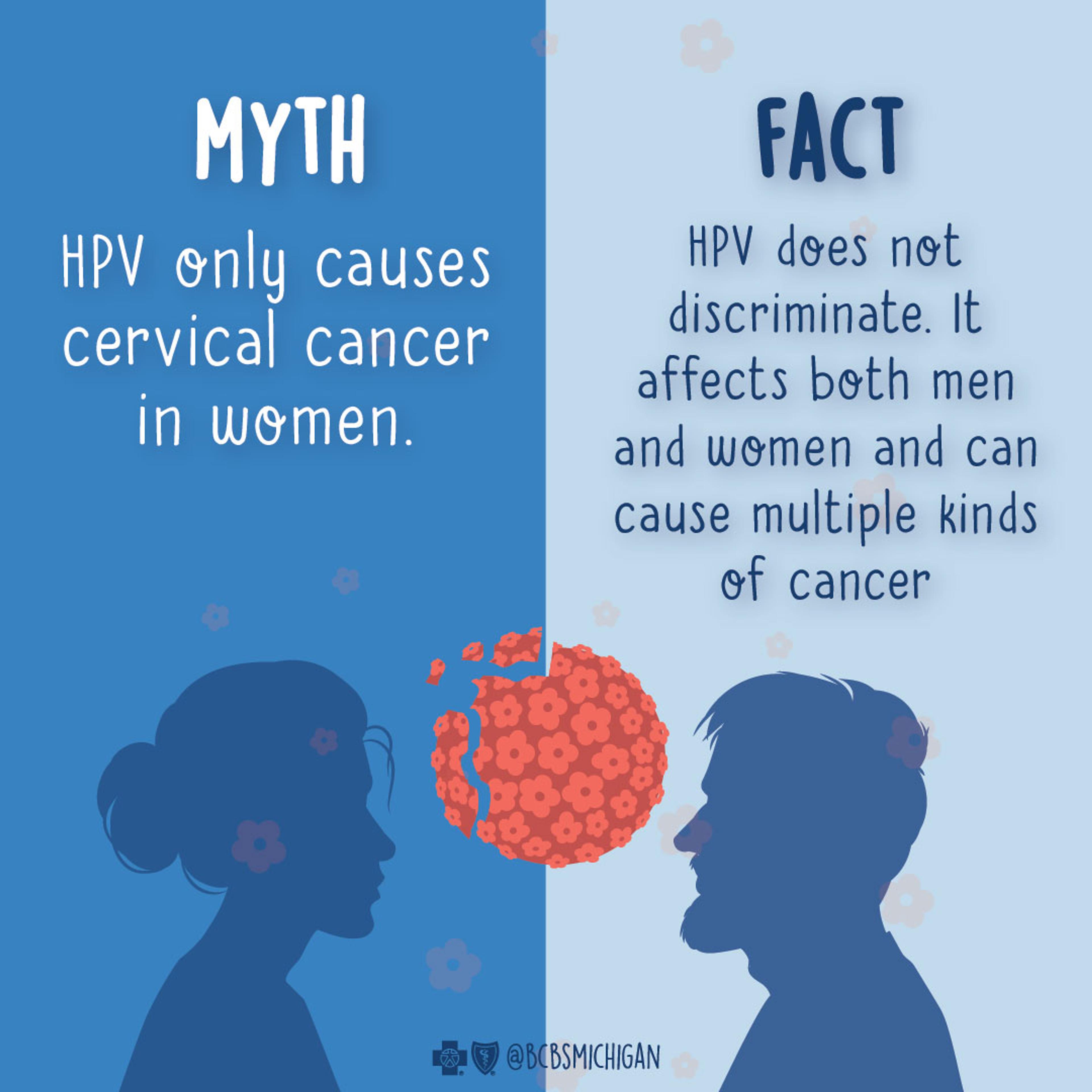
Myth: HPV only causes cervical cancer in women.
Fact: HPV does not discriminate. It affects both men and women and can cause multiple kinds of cancer:
- In men and women, HPV can lead to genital warts, anal cancers, and cancers of the mouth, throat, head and neck.
- In women, HPV can lead to cervical cancer, as well as vaginal and vulvar cancer.
Myth: The HPV vaccine causes fertility issues.
Fact: The HPV vaccine does not cause fertility problems. More than 135 million doses have been distributed in the U.S. since the HPV vaccination was first released. The Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration continually monitor vaccines for safety issues and have not found that the vaccine increases the risk of fertility problems in women or men.
However, not receiving the HPV vaccine does increase the risk of a woman developing cervical cancer or precancer. The therapy necessary to treat these cancers and precancers can influence a woman’s ability to become pregnant or carry a pregnancy to full term. In this way, the HPV vaccination can help preserve fertility.
Myth: Only people who are sexually active will need the HPV vaccine.
Fact: The HPV vaccination is most effective when given to adolescents before they become sexually active. Therefore, the CDC recommends that everyone is vaccinated prior to sexual activity. Receiving the vaccine as an adolescent is not linked to earlier sexual activity.
Health experts at the CDC recommend girls and boys receive the HPV vaccine between the ages of 11 and 12 – and it can be administered as early as age 9.
It is still recommended for all men and women who have not been fully vaccinated and are 26 years of age and younger, to receive the vaccination. For patients aged 27-45, it is recommended to have a shared decision-making visit with your physician to decide if you need to be vaccinated based on your risk of HPV infection.
Myth: The HPV vaccine only prevents genital warts.
Fact: The HPV vaccine does prevent genital warts, but it also prevents cancer in both men and women.
Individuals should talk with their health care provider if they have questions about the HPV vaccine.
Martha Walsh, M.D., is a senior medical director and associate chief medical officer at Blue Cross Blue Shield of Michigan.
Photo credit: Getty Images






