2023 Blue Care Network Annual Report: Delivering affordable and convenient health care that’s easy, useful and personal

Blue Daily
| 3 min read

A MESSAGE FROM THE PRESIDENT AND CEO, BLUE CROSS BLUE SHIELD OF MICHIGAN
“Blue Care Network is driven by our values as a nonprofit mutual company and our historic commitment to Michigan’s communities. As the state’s largest health maintenance organization, Blue Care Network is ready to help our customers and members get the best care possible with comprehensive health care coverage.”
A MESSAGE FROM THE PRESIDENT AND CEO, BLUE CARE NETWORK
“We know members count on us during critical moments. So we aim to make health care less complicated. With this in mind, Blue Care Network introduced innovative health care solutions that are not only cost-efficient, but deliver easy, useful and personal experiences to our members.”
A MESSAGE FROM THE CHAIR, BLUE CARE NETWORK BOARD OF DIRECTORS
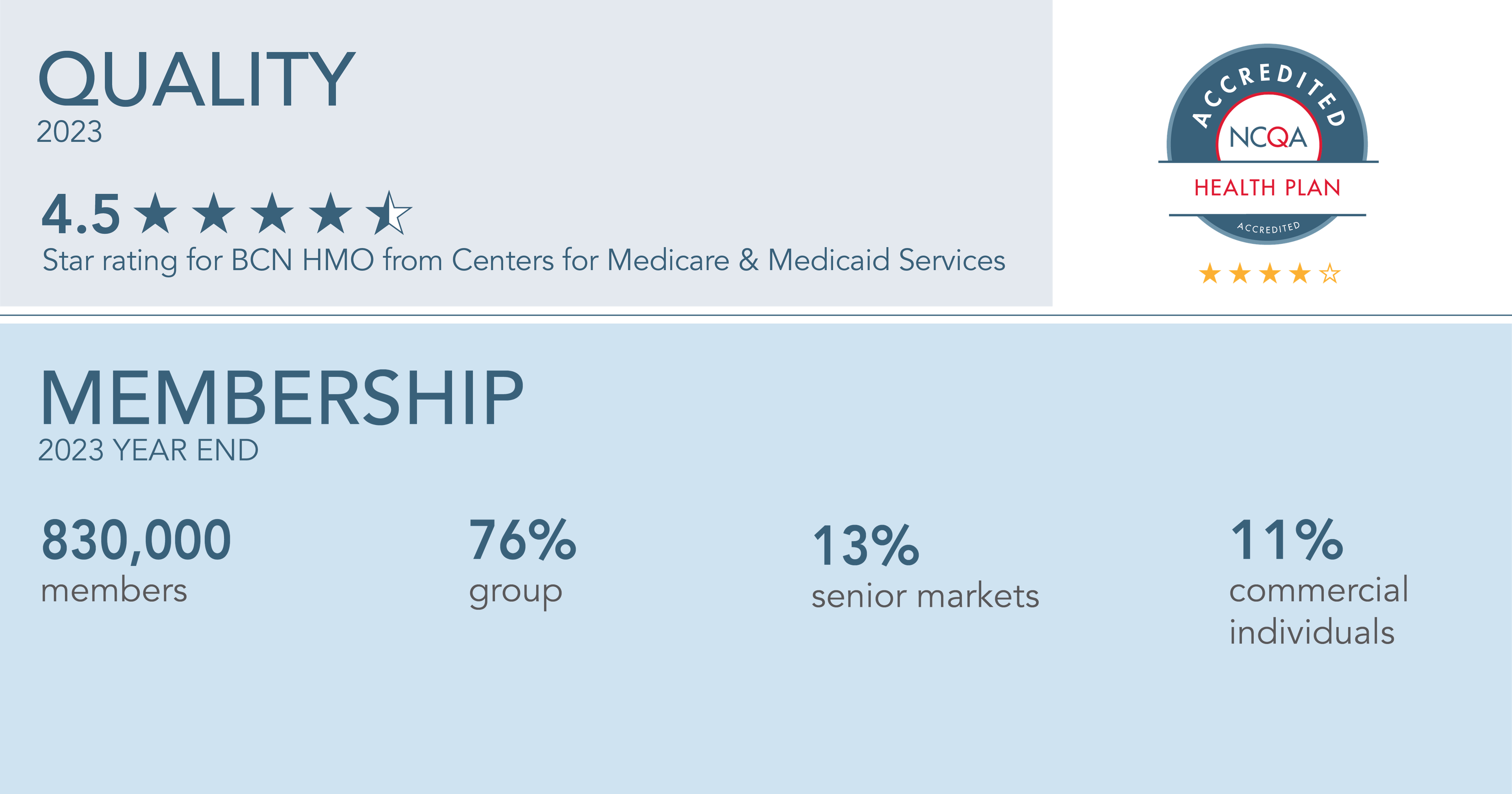
“In 2023, Blue Care Network maintained strong membership levels of close to 830,000 and 40% of the Michigan HMO market. We continue to help our members manage cost savings while delivering a diverse and dynamic portfolio of health care choices.”
A YEAR IN REVIEW: 2023 HIGHLIGHTS
Blue Care Network is ready to help with easy, useful and personalized health care options. In 2023, we developed new programs and services with built-in convenience and more affordability to deliver quality care to our customers, members and communities.
DELIVERING HIGH-QUALITY, COST-SAVING PHARMACY SERVICES
- Introduced Price Edge, a service that automatically finds the lowest price available on medications when BCN members fill their prescriptions, resulting in savings of over $1.8 million in out-of-pocket costs from 248,000 claims.
- Launched our newest free adherence pilot program, Generics Advantage Program. BCN members receive discounts on select generic medications and save money on out-of-pocket costs when they adhere to their drug therapies.
- Generated more than $3.9 million in savings for BCN members on specialty and other expensive drugs through our High-Cost Drug Discount Optimization Program.
- Produced nearly $3.1 million in savings for BCN and Blue Cross members with chronic conditions enrolled in our Drug Adherence Discount Program.
- Helped BCN members experience cost savings through a pharmacy partnership that lowered prescription drug prices on the top 15 medications.
- Expanded our Personalized Medicine program to 150,000 eligible BCN members with pharmacy benefits in January 2023, following favorable medical and drug cost reductions for members who participated in the 2022 pilot program.
DELIVERING AFFORDABLE AND CONVENIENT HEALTH CARE THAT’S EASY, USEFUL AND PERSONAL
- Launched a two-year diabetes remission pilot program that combines artificial intelligence with an easy-to-use app and personal guidance from a health coach to help members with Type 2 diabetes lower their A1c, reduce medications and lose weight.
- Expanded our Family Building and Women’s Health Support Solution to include a new personalized digital care app to guide members through a healthy transition into menopause.
- Expanded crisis services to eight crisis care centers across Michigan to help members get urgent care for behavioral health concerns.
- Completed 139 field service visits, including virtual and in-person educational sessions and open enrollment support, to help customers deliver better plan understanding to their members.
- Launched the Estimate Your Cost tool to help members with commercial plans understand their treatment costs and provide them with personalized, out-of-pocket estimates for covered health care items and services.
CONTINUING OUR COMMITMENT TO OUR COMMUNITY
See how we partner with our parent company, Blue Cross Blue Shield of Michigan, to better support health and wellness initiatives in the communities we serve in the 2023 Community Outreach Annual Report.
Learn more about enterprise-wide efforts to recognize the diverse health care needs of our members and communities in the 2023 Inclusion and Diversity Annual Report.